Health sector policies
Ebola: How decent work in the health sector saves lives of health personnel
International labour standards and tools, if correctly applied, are very effective in protecting frontline health workers treating patients with potentially deadly infectious diseases, such as Ebola, says Christiane Wiskow, Senior Health Sector Specialist at the International Labour Organization (ILO).
 |
| Christiane Wiskow, Senior Health Sector Specialist at the ILO |
The report, Health worker Ebola infections in Guinea, Liberia and Sierra Leone: A preliminary report, (WHO, 21 May 2015) states that 815 confirmed and probable cases of Ebola-infected health workers were reported in Guinea, Liberia and Sierra Leone during the period January 2014 to March 2015. Two thirds of those health workers (for whom a final outcome is known) died of Ebola. For some health-related occupations, the risk of infection is 21 to 32 times higher than for the general population.
More than half of the infected health workers were nurses and nurse aides. Other categories of health workers affected included medical workers (12 per cent); laboratory workers and support staff (e.g. janitors and maintenance staff, seven per cent each). These work-related infections could largely have been prevented.
Action towards safe working conditions needed
Assertive global action on safe working conditions for health workers is needed to ensure that this terrible toll is not repeated in controlling the next outbreaks of deadly communicable diseases.
The ILO strongly advocates for ensuring health workers’ safety and health, including through the use of its standards and tools developed specifically for the purpose.
ILO tools and standards protect health workers
Here are some examples that illustrate the relevance of ILO tools and standards in protecting health workers:- In Liberia, the Ministry of Health and WHO used HealthWISE, a joint ILO/WHO participatory action and learning tool, to train health workers in improving workplace safety during the outbreak. The HealthWISE action checklist has been adapted to the context of Ebola in Liberia: it guides health facilities to check and establish procedures for infection prevention and control (IPC) and occupational safety and health (OSH). These include procedures for cleaning and disinfecting equipment, hand hygiene, proper use and maintenance of personal protective equipment (PPE) and a system for monitoring and reporting on staff health, such as daily temperature checks.
- A 2014 ILO/WHO briefing note Ebola Virus Disease: Occupational Safety and Health reminds employers of their responsibilities to ensure workers’ safety and health by providing information, training and PPE to prevent occupational infection and other safety and health incidents. It also affirms workers’ responsibilities to comply with regulations.
- Along with ILO OSH standards, the ILO Nursing Personnel Convention, 1977 (No. 149) and its accompanying Recommendation 157 provide guidance on appropriate conditions of work for nursing personnel. These instruments stipulate that OSH laws and regulations should be improved by adapting them to the special nature of nursing work and of the environment in which it is carried out (C 149, Article 7). With a total of 41 ratifications, Convention 149 was ratified by Guinea in 1982, but not yet by Liberia or Sierra Leone.
Supplies, IPC and OSH critical
At the onset of the Ebola outbreak in the three most affected West African countries, health personnel faced a dire lack of PPE, according to a 2014 Public Service International survey.The WHO report confirms that infection rates of health workers were highest at the beginning of the outbreak and peaked in August 2014. This suggests that implementing IPC measures and OSH strategies, in addition to using safe supplies, when they became available, contributed to the reduction of health worker infections.
Number of confirmed and probable health worker EVD cases over time (and proportion of health worker cases among all cases* reported) in the three countries combined (Guinea, Liberia and Sierra Leone), 1 January 2014 - 31 March 2015
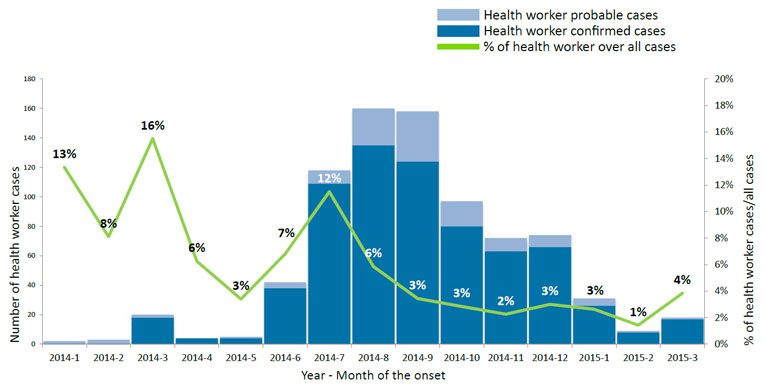
* All cases include health worker and non-health worker confirmed and probable cases.
Ebola-infected health workers without hospitalization died at higher rates than those with hospital treatment (74 per cent compared to 61 per cent), according to the WHO report. Some survivors are struggling, not only with chronic pain, headaches and eye trouble but also with stigma and discrimination in their communities. Many have been traumatized and need psycho-social support. Like all people affected by Ebola, health workers and their families need comprehensive social protection measures that address the consequences of the disease, including loss of income, in the short- and long-terms.
Decent work saves lives
Health workers treating patients with potentially deadly diseases should not have to put their lives unduly at risk in the course of duty. Health-care settings with effective OSH management systems, in addition to well-informed and trained employers and workers who have the necessary medical equipment and supplies are critical in minimizing risks. A protected and supported health workforce is essential in providing effective care, particularly in emergency situations.The United Nations Secretary-General has convened an International Ebola Recovery Conference in New York from 9-10 July 2015